The Importance of Primary Care
A recent study by The Commonwealth Fund Commission estimated that up to 150,000 lives and $100 billion dollars could be saved annually if primary health care reached higher performance levels¹.
More than two decades of accumulated evidence has revealed that having a primary care physician:
- Reduces illness days and deaths caused by cardiovascular and pulmonary diseases
- Decreases use of emergency departments and hospitals
- Improves preventive care
- Improves detection of breast cancer
- Reduces the incidence and mortality caused by colon and cervical cancer
- Fewer tests, higher patient satisfaction, less medication use, and lower care-related costs
- Reduces health care inequalities, particularly for populations with wide income variation, including improved vision, more complete immunization, better blood pressure control, and better oral health²
Yet, in the United States of America, while leading the world in total per capita health care spending, we lag behind nearly all other industrialized nations in quality of primary care services and suffer accordingly with high rates of preventable diseases.
Not surprisingly, as support for primary care services in this country has fallen, fewer doctors in training are choosing to become Family Physicians, General Internists and Pediatricians, the primary care specialists. The American Academy of Family Practice and the Institute of Medicine have predicted a collapse of primary care if changes do not occur³. We appear to lack the political will to reorient our health system to primary care and to provide coverage and access to health care for all America.
The Planned Care Model
However, the news in primary care is not all bad. Despite the stresses, and perhaps in part because of them, primary care physicians have been forced to reevaluate their work and to determine its true value to those that they serve, their patients. A new focus on quality with measurable improvements in health outcomes is driving physicians and health systems to define a “New Model of Care” that is patient-centered, safe, timely, effective, equitable, and efficient.
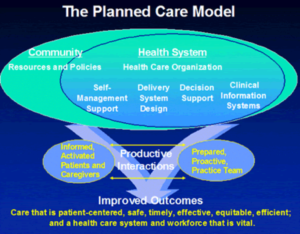
A pioneer in this effort, Dr. Ed Wagner, M.D., has described “The Planned Care Model”. This model of care, developed with the support of The Robert Wood Johnson Foundation and the MacColl Institute for Healthcare Innovation identifies the essential elements of a health care system that encourage high-quality care. These elements are the community, the health system, self-management support, delivery system design, decision support and clinical information systems.
North Olympic Healthcare Network (NOHN) has embraced the planned care model while pioneering the use of the electronic health record on the North Olympic Peninsula. We have been measuring and improving the health statistics of the thousands of patients we care for and are redesigning our clinic to continue to provide measurable improvements in care. These changes are designed to streamline the process of care while fulfilling our mission: To provide our patients with the highest quality primary care in the world.
We are dedicated to a clinical model that brings informed, activated patients in contact with a prepared, proactive practice team to have productive interactions and improved health outcomes, as envisioned in the planned care model.
What characterizes an “informed, activated” patient?
- He or she understands the disease process, and recognizes his/her role as the daily self-manager.
- Family and caregivers are engaged in the patient’s self-management.
- The physician is viewed as a guide on the side, not the sage on the stage.
What characterizes a “prepared, proactive” practice team?
- At the time of the visit the people, patient information, equipment, decision support, and time are available to deliver evidence-based care and self-management support.
What can we expect from a “planned care” model?
- Productive interactions in the primary care setting translate into fewer cancers, fewer chronic diseases such as diabetes, and decreased catastrophic events such as heart attacks and strokes. Feeling better and living longer in a state of good health are goals we can work towards together.
At NOHN, we seek to provide our patients with a medical home where their health care needs are addressed efficiently and with high quality.
Sources:
² American Family Physician, August 1, 2004 by Robert L. Phillips, Jr., Barbara Starfield.